Panic Protocol
This protocol for panic disorder is built on core interventions. It can be conducted both online and in a blended manner, and is based on existing protocols, scientific sources, and mental health care standards, using NiceDay. In this treatment, you emphasize strengths, build trust, and encourage an active work attitude. Additionally, you facilitate autonomy through encouragement and motivation, collaborative decision-making, and involving loved ones. Based on your client's personal situation and complaints, you can utilize supportive articles, with inspiration provided at the end of the protocol.
This protocol provides therapists with guidance and inspiration on the possibilities within NiceDay. The protocol is structured around core interventions that can be applied based on the therapist's assessment. The protocol does not need to be strictly followed; rather, it can be adapted to fit the client's situation and complaints.
Core interventions
The CBT treatment for panic consists of the following core interventions:
🧪Thought records and behavioural experiments
🧘Other interventions in case of panic
- Relaxation- and/or breathing exercises can be used as part of panic management to reduce or tolerate tension, for example. These exercises can serve not only during panic episodes (in which case they might become safety behaviours) but also as general skills.
- Pharmacological therapy can be considered in addition to the CBT treatment, based on consultation and agreement with the client.
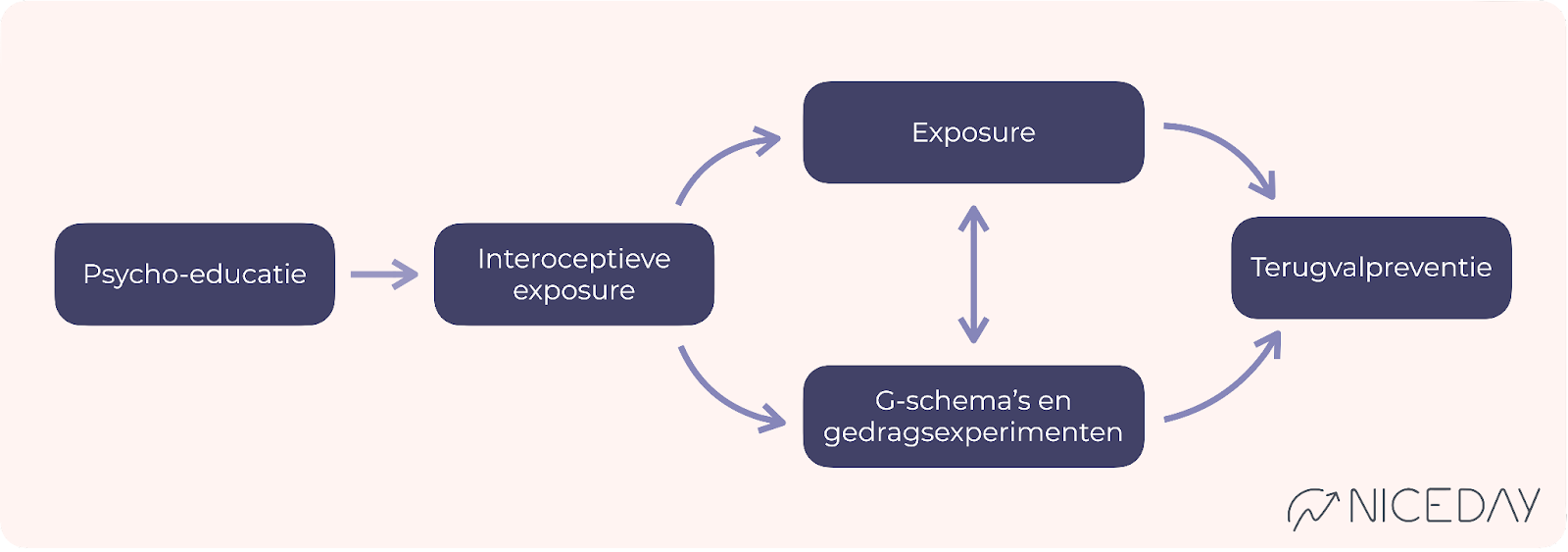
The sequence
The treatment begins with psychoeducation about panic, anxiety, and CBT. This is followed by interoceptive exposure exercises. Afterward, as a therapist, you can decide whether to proceed with in vivo exposure or cognitive therapy (using thought records and behavioural experiments). The treatment concludes with relapse prevention.
The pace and frequency
Depending on the severity of the symptoms and the effectiveness of the therapy, you can expect the duration to be approximately 8 to 20 sessions. The recommendation is to schedule frequent sessions at the beginning of the treatment. It is important, in terms of managing expectations, to make agreements with your client regarding the duration of the treatment.
Outcome Feedback (OMQ and SMQ)
To monitor progress effectively, you can use two short (5-question) questionnaires that are administered around each session. Prior to each session, the Outcome Measurement Questionnaire (OMQ) assesses the severity of the symptoms. After each session, the Session Measurement Questionnaire (SMQ) evaluates the quality of the treatment session and the working relationship. You can find the manual here. If necessary, discuss the results with your client.
Flexible Time
Flexible time refers to the time you spend with your client outside of the sessions (e.g., chatting, sending psychoeducation, or writing session notes). This allows you to stay engaged with your client and monitor progress effectively. You can assess how much time is needed per client. If you need more inspiration for what you can do, refer to this article.
Within the flexible time there are a number of standard actions per session:
|
Involving Social network
Discuss with your client whether and how their social network can be involved in the treatment process. The client's environment can both facilitate and unintentionally hinder the treatment process by maintaining avoidance and safety behaviours. You can find information on how to involve the social network in the treatment process here.
📖 Core Intervention Psychoeducation
The goal of Psychoeducation is to provide your client with an explanation about panic and to prepare them for one of the following core interventions by starting with symptom registration. This typically takes around 1-2 sessions.
Deepening core intervention: Psychoeducation
Flexible time - prior to the first session: 5 minutes Welcome message
Psychoeducation
|
Session (1 or 2 sessions) 35 min
What can you do?
- Explain outcome feedback (OMQ and SMQ).
- Discuss the psycho-education and check for questions.
- Work together with the client to define the treatment goals.
- Explore the possibility of involving the client's social network in the treatment.
- Co-create SMART treatment goals and establish crisis plans if needed.
- Together, map out the panic cycle.
- As a logical continuation, discuss safety behaviours and avoidance.
- Activate trackers:
Panic Attacks, Safety Behaviours, Anxiety and Avoidance
This will help in mapping out safety behaviours and avoidance in preparation for the next sessions. - Explain to your client the importance of tracking panic attacks, avoidance, and safety behaviours.
- Plan the next session(s) with your client. Turn on OMQ and SMQ.
- Provide examples of exercises and assignments for them to do at home:
- Ask your client to create a session note and explain how to do it.
- Encourage your client to read the provided psycho-education if they haven't done so already.
- Share psycho-education about anxiety with their loved ones.
- Ask your client to fill out the SMQ after the session.
Flexible time: 15 min How can you fill this time during the week?
|
🔎 Interoceptive exposure
The goal of Interoceptive Exposure is to expose the client to bodily sensations associated with a panic attack. You practice together initially and then have the client practice alone, aiming to reduce the fear of these bodily sensations. This core intervention continues until the fear subsides completely and can be extended through the end of the treatment if necessary.
In-depth explanation of the core intervention Interoceptive Exposure.
Flexibele tijd - vóór de eerste sessie over exposure 5 min
|
Session 1 35 mins
- Go through the homework together and evaluate avoidance and safety behaviours.
- Explain exposure. Do the interoceptive exposure exercise together during the session and evaluate the experiences.
- Discuss the exercises and assignments for home:
- Practice the interoceptive exposure exercise(s) two to three times daily and record it
- Ask your client to continue recording panic attacks, avoidance, and safety behaviours
Flexible time: 20 min
|
After interoceptive exposure, you can proceed with either in vivo exposure or cognitive therapy (Thought records & behavioural experiments), depending on your client's progress. It's important to continue with interoceptive exposure exercises simultaneously until the desired outcome is achieved.
🔥 Core Intervention Exposure in vivo
The goal of Exposure is to expose your client to anxiety-provoking situations. You collaborate to identify situations that are being avoided and then guide your client through repeated practice of facing these situations. This typically takes at least 4 sessions.
Deepening the Core Intervention of Exposure in vivo
Flexible time - before the first exposure session 5 min
|
Session 1 35 mins
- Briefly assess how the interoceptive exposure exercises are progressing, and then relate them to in vivo exposure.
- Explain exposure again if necessary. Collaboratively identify with your client which situations and activities are being avoided or endured with high tension. You can also refer to the recorded safety behaviour and/or avoidance for this purpose.
- Choose an anxiety-provoking situation to practice together with your client. This situation should be challenging but manageable.
- Plan the exposure exercise together on NiceDay and ask about the anxious "if-then" expectations.
- Examples of exercises and assignments for home:
- Perform the agreed-upon exposure exercise.
- Record a list of anxious situations in the diary.
- Continue recording panic attacks, avoidance, and safety behaviour.
Flexible time: 20 min
|
Session 2 to 4: 30 min
- Assess how the (interoceptive) exposure exercises are progressing.
- Review the list of anxious situations together and agree that the client will do one exposure exercise from the list daily over the next week.
- Schedule which exercise will be done when, or let the client plan it themselves.
- Continue discussing the results of all activated trackers.
- Discuss the exercises and assignments for home:
- Schedule the agreed-upon exposure exercises, carry them out, and record how they went.
- Continue filling out the activated trackers, including panic attacks.
Flexible time: 20 min
|
🧪 Core Intervention Thought records and Behavioural Experiments
The purpose of Thought records and Behavioural Experiments is to examine and test the role of unhelpful thoughts in unwanted feelings or behaviours against reality. You assess and challenge unhelpful thoughts using the Thought records and create behavioural experiments to engage in new behaviour in practice. On average, this takes at least 6 sessions.
Deepening core intervention Thought records
Deepening core intervention behavioural experiments
Flexible time - before the first session: 5 min
|
Session 1: 35 mins
- Assess how the interoceptive exposure exercises are progressing.
- Check if there are any questions about the shared psycho-education.
- Explain the influence of anxious cognitions using personal examples, such as the most recent panic attack.
- Use the Socratic method to explore what the anxious cognitions related to panic-inducing situations are.
- Fill out step 1 of the Thought record together in NiceDay. Verify with your client if the Thought record is clear.
- Examples of exercises and assignments for home:
- Complete step 1 of the Thought record for anxiety-provoking situations.
- Ask your client to continue tracking panic attacks, avoidance, and safety behaviours.
Flexible time: 20 min
|
Session 2: 35 min
- Assess how the interoceptive exposure exercises are progressing.
- Discuss the exercises and assignments that have been done at home, and evaluate step 1 of the Thought record together with the client.
- Introduce steps 2 and 3 of the Thought record through psycho-education about challenging thoughts in a Thought record. Then, you can proceed to challenge a thought together using a previously filled Thought record.
- Provide explanations about thinking styles if necessary.
- Examples of exercises and assignments for home:
- Fill in steps 1 through 3 of the Thought record for anxious situations.
- Ask your client to set a daily reminder for the Thought record.
- Request your client to continue recording panic attacks, avoidance, and safety behaviour.
Flexible time: 20 min
|
Session 3: 35 min
- Assess how the interoceptive exposure exercises are progressing.
- Discuss the exercises done at home and encourage your client to continue filling out the Thought records.
- Discuss the helpful thoughts and insights gained together. Use this as a bridge to the behavioural experiments.
- Review the summary of the recorded number of panic attacks, avoidance, and safety behaviours in the graphs on NiceDay to discuss the impact of the interventions.
- Provide an explanation about behavioural experiments.
- Explain why it's important to start experimenting with different behaviour from now on. Ask what someone else would do if they were to act based on these new helpful thoughts.
- You can also choose to use the recorded safety behaviours and/or avoidance as inspiration for behavioural experiments.
- Collaboratively create a first behavioural experiment and schedule it in NiceDay.
- Examples of exercises and assignments for home:
- Keep practicing steps 1 through 3 of the Thought record.
- Execute the behavioural experiment and record it in NiceDay.
- Continue recording panic attacks, avoidance, and safety behaviours.
Flexible time: 20 min
|
Session 4 to completion: 35 min
- Assess how the interoceptive exposure exercises are progressing.
- Discuss how the first behavioural experiment went.
- Encourage your client to continue filling out the Thought records.
- Collaboratively come up with more experiments for your client to practice (preferably as many as possible).
- Examples of exercises and assignments for home:
- Keep filling out Thought records.
- Carry out the behavioural experiments and record them in NiceDay.
- Continue recording panic attacks, avoidance, and safety behaviours.
Flexible time: 20 min
|
Evaluate the effectiveness of the Thought records and behavioural experiments, along with the insights gained, after 5 sessions. If the intervention is effective, continue until the new cognitions and behaviours are more or less 'anchored' and the treatment goals are (largely) achieved. If you notice that the therapy is not yielding sufficient results despite the efforts of both you and the client, discuss this with the client and in the multidisciplinary team (MDT) meeting. Explore potential reasons and adjust the therapy if necessary.
🔁Core intervention Relapse prevention
The goal of Relapse Prevention is to map out how someone can identify and monitor potential relapses, identify their pitfalls, and provide tools to manage symptoms or situations. This typically takes 1-2 sessions.
Deepening core intervention relapse prevention
Flexible time - before the first session on relapse prevention: 5 minutes.
|
Session (1 or 2 sessions) 35 min
- Reflect on the progress of the OMQ and SMQ and discuss any other (ROM) questionnaires if applicable.
- Evaluate the treatment:
- Discuss the effect of the treatment.
- Which obstacles have been overcome, and which ones are still present?
- Predict and normalize: It is normal to experience anxiety again in the future. Stress, fatigue, and/or changes in your life can play a role in this.
- Collaboratively create the relapse prevention plan:
- Create a list of situations and problems where the risk of falling back into old behaviours exists.
- Have your client write down a strategy for each situation that can be applied in those specific circumstances.
- Exercises and assignments for home:
- Encourage your client to continue applying everything that has been learned. Also, remind them to keep using the app, such as filling out trackers to stay aware of the frequency of panic attacks, avoidance, and safety behaviours, and using the Thought record to challenge unhelpful thoughts.
- Ask your client to complete the relapse prevention plan.
Flexible time: 20 min
|
📚 Extra articles
Based on your client's personal situation and issues, you can utilize supportive blogs. These are written by professionals and individuals with relevant experiences and can be found on niceday.app. Consider topics such as:
- Affirmations against your anxious thoughts
- Are you a control freak? Learn to let go of control!
- No panic! This is how you prevent a panic attack.
- Fear about fear.
- Feeling mentally tense...? Try physical relaxation!
- Thinking patterns with anxiety.
- Four tips for improving self-esteem.
- Insecure: 6 tips!
- Living with uncertainty.
- Avoidance: short-term relief for your long-term issues.
- Catastrophic thinking.
Sources
- https://www.ggzstandaarden.nl/zorgstandaarden/angstklachten-en-angststoornissen/introductie
- Kampman, M., Keijsers, G. & Hendriks, G., Protocollaire behandeling van patiënten met een paniekstoornis met of zonder comorbide agorafobie. In: Keijsers, G. P. J., Van Minnen, A., Verbraak, M., Hoogduin, C. A. L. & Emmelkamp, P., (2021). Protocollaire behandelingen voor volwassenen met psychische klachten.
- Sánchez-Meca J, Rosa-Alcázar AI, Marín-Martínez F, Gómez-Conesa A. Psychological treatment of panic disorder with or without agoraphobia: a meta-analysis. Clin Psychol Rev. 2010 Feb;30(1):37-50.
- Pompoli A, Furukawa TA, Efthimiou O, Imai H, Tajika A, Salanti G. Dismantling cognitive-behaviour therapy for panic disorder: a systematic review and component network meta-analysis. Psychol Med. 2018 Sep;48(12):1945-1953.