Depression Protocol
This protocol for depression is composed of core interventions. It can be delivered both online and in a blended format and is based on existing CBT protocols, scientific sources, and mental healthcare standards, using NiceDay. Within this treatment, the emphasis is on strengths, increasing confidence, and promoting an active work attitude. Autonomy is facilitated through encouragement and motivation, shared decision-making, and involvement of significant others. Supportive articles can be used based on the client's personal situation and complaints, and sources of inspiration for these are provided at the end of the protocol.
This protocol provides therapists with guidance and inspiration regarding the possibilities within NiceDay. The protocol consists of core interventions that can be implemented based on the therapist's assessment. It does not have to be strictly followed, but can be tailored to the client's situation and complaints.
Core interventions
The CBT treatment for depression consists of the following core interventions:
🧪 Thought records and behavioural experiments
💊 In consultation, pharmacological therapy can be used as an adjunct to CBT treatment
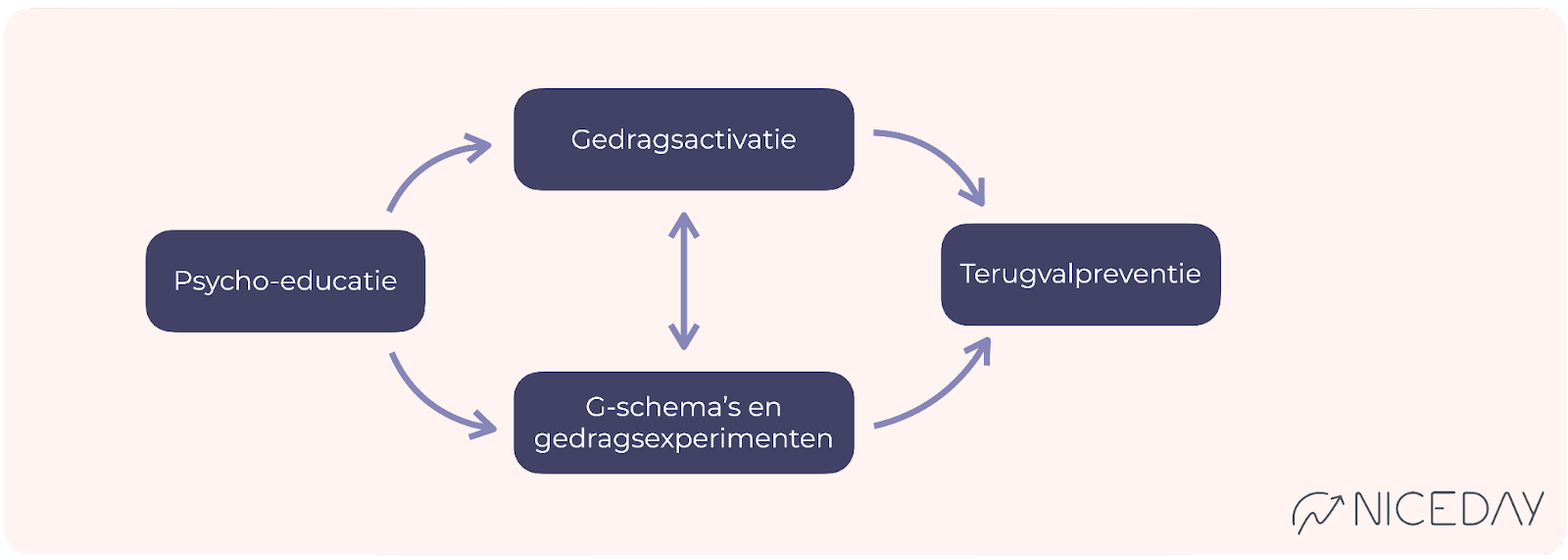
The sequence
The treatment begins with psycho-education about depression and CBT. The recommendation is to then proceed with behavioural activation. Depending on your client, you determine how many sessions to dedicate to this. If behavioural activation is insufficiently effective, you can transition to cognitive interventions. Behavioural activation should ideally be incorporated in every session. The treatment always concludes with relapse prevention.
The pace and frequency
Depending on the severity of the symptoms and the effectiveness of the therapy, you can expect the duration to be approximately 8 to 20 sessions. The recommendation is to schedule frequent sessions at the beginning of the treatment. It is important, in terms of managing expectations, to make agreements with your client regarding the duration of the treatment.
Outcome Feedback (OMQ and SMQ)
To monitor progress effectively, you can use two short (5-question) questionnaires that are administered around each session. Prior to each session, the Outcome Measurement Questionnaire (OMQ) assesses the severity of the symptoms. After each session, the Session Measurement Questionnaire (SMQ) evaluates the quality of the treatment session and the working relationship. You can find the manual here. If necessary, discuss the results with your client.
Flexible Time
Flexible time refers to the time you spend with your client outside of the sessions (e.g., chatting, sending psychoeducation, or writing session notes). This allows you to stay engaged with your client and monitor progress effectively. You can assess how much time is needed per client. If you need more inspiration for what you can do, refer to this article.
Within the flexible time, there are several standard actions per session:
|
Involving Social network
Discuss with your client whether and how their social network can be involved in the treatment process. The client's environment can both facilitate and unintentionally hinder the treatment process by maintaining avoidance and safety behaviours. You can find information on how to involve the social network in the treatment process here.
📖 Core Intervention Psychoeducation
The goal of Psycho-education is to provide your client with information about social anxiety and prepare them for one of the core interventions by initiating symptom monitoring. This typically takes about 1-2 sessions on average.
Deepening core intervention psycho-education
Flexible time - prior to the first session 5 min Send welcome message
Sharing Psychoeducation
|
Session (1 or 2 sessions) 35 min
What can you do?
- Provide an explanation of outcome feedback (OMQ and SMQ).
- Discuss psycho-education and check for any questions.
- Collaboratively discuss the treatment goal.
- Discuss the potential involvement of the social network in the treatment.
- Together, establish SMART treatment goals and potentially create crisis agreements. If there is a presence of suicidality, it is important to monitor this on a weekly basis.
- Map out the vicious cycle of behaviour together.
- Emphasize the importance of activation and a healthy lifestyle.
- In consultation with the client,
Activate trackers such as Check In (mood registration), Energy, Exercise,
or other relevant trackers such as: Feelings of depression, Loneliness, Sadness - Plan the next session(s) in consultation with the client. Activate the OMQ and SMQ.
- Examples of exercises and assignments to do at home:
- Activity Log: Ask your client to record activities in a diary and categorize them as "must" or "pleasurable" activities.
- Mood Logging: Ask your client to fill in their mood for each activity they engage in.
- If needed, provide the list of enjoyable activities to get an idea of enjoyable activities and to inspire your client.
- Ask your client to engage in and register one activity.
- Ask your client to create a session note and explain how to do it.
- Share psychoeducation about depression with the client's loved ones.
- Ask your client to fill out the SMQ after the session.
Flexible time 15 min How can you occupy this time during the week?
|
⏯️ Core Intervention: Behavioural Activation
Behavioural Activation aims to promote positive reinforcement and improve mood by engaging in more activities. You explore the effect of various activities such as sports or social interactions on mood and gradually expand upon them. This can be continued until the end of the treatment, but at least 3 sessions are recommended.
Deepening Core Intervention: Behavioural Activation
Flexible Time - Before the first session on behavioural activation, allocate 5 minutes.
|
Session 1: 35 mins
- Review the registrations together and discuss the insights gained. If necessary, refer back to the vicious cycle of behaviour.
- Based on the activity log, make adjustments to the daily structure to increase pleasurable activities and/or reduce must-do activities. Schedule these activities in NiceDay or have your client do so. Motivate your client to follow through with these plans.
- Ask, if relevant, whether there are any activities on the list of pleasurable activities that your client would like to integrate into the new structure.
- Tip! You can integrate lifestyle interventions with pleasurable activities.
- Discuss whether the client wants to engage in more physical activity. If yes, you can activate the Step Tracker and make agreements about a step goal.
- Examples of exercises and assignments for home:
- Engage in fewer obligatory activities and more pleasurable activities.
- Follow the new daily structure.
- Complete the Trackers and Check-In.
- Ask the client to make a session note of this session.
Flexible time 20 min
|
Session 2: 35 mins
- Review the registrations together and discuss the insights gained. You can also refer back to the vicious cycle of behaviour if necessary.
- Expand the activation goals if possible. Pay particular attention to whether pleasurable activities can be increased or obligatory activities can be reduced.
- If there are repeated unsuccessful activities, you may choose to explore this together using a Situation-Behaviour-Consequence (SBC) schema or a functional analysis.
- Examples of exercises and assignments for home:
- Schedule, carry out, and register the agreed-upon goals.
- Fill in the trackers and mood registration.
Flexible time 20 min
|
Session 3 to the last session 35 min
Whether to continue with behavioural activation and in what form depends on the client's progress and goals.
- If behavioural activation has insufficient effect, you can discuss this in your supervision or consultation with peers. There are additional options to increase the likelihood of success (such as stimulus control, skill training, involving the social environment, identifying life goals), or you can choose to switch to cognitive interventions.
- If behavioural activation has the desired effect for the client, you can continue with it. The treatment goals should guide your decision. You can consider whether the cognitive component is still necessary. Discuss this with your client and/or in supervision or consultation.
- If there are inhibiting cognitions, you can proceed to the section on cognitive schemas and behavioural experiments. If behavioural activation is effective, continue with it during the cognitive interventions.

🧪 Core Intervention Thought records & Behavioural Experiments
The goal of Thought Records and Behavioural Experiments is to examine and test the impact of unhelpful thoughts on unwanted emotions or behaviours, and evaluate them based on reality. You identify and challenge unhelpful thoughts using Thought Records, and design behavioural experiments to practice new behaviours. On average, this process takes at least 6 sessions.
Deepening core intervention thought record
Deepening core intervention behavioural experiment
Flexible time - before first Cognitive Therapy session 5 min
|
Session 1: 35 mins
- Explain the purpose of Cognitive Therapy.
- Complete - if desired - the Cognitive Model together.
- Fill in Step 1 of the Thought record together.
- If behavioural activation has been successful, continue with it.
- Examples of exercises and assignments for home:
- Fill in Step 1 of the Thought record daily. Set a reminder.
Flexible time 20 min
|
Session 2: 35 mins
- Discuss the homework and monitor if the client understands everything. Provide additional explanations about feelings, thoughts, and behaviour if necessary.
- Review step 1 of the completed Thought records together and explore common unhelpful thoughts. Then, fill out steps 2 and 3 together with your client.
- Monitor the continuation of behavioural activation.
- Examples of exercises and assignments for home:
- Fill out a Thought record daily (steps 1 to 3). Set a reminder.
- Practice challenging unhelpful thoughts.
- Practice formulating helpful thoughts.
Flexible time 20 min
|
Session 3: 35 mins
- Discuss the homework and monitor whether your client understands everything.
- Review the Thought records and discuss non-helpful and helpful thoughts.
- Provide support, if necessary, in formulating helpful thoughts. You can also use other cognitive techniques for this purpose.
- Discuss possible existing thinking styles together.
- Monitor the continuation of behavioural activation.
- Examples of exercises and assignments for home:
- Fill out a Thought record daily, optionally with a reminder.
- Practice challenging unhelpful thoughts and formulating helpful thoughts.
- Practice recalling or remembering helpful thoughts.
- Practice recognizing thinking styles.
Flexible time 20 min
|
Session 4: 35 mins
- Examine - if relevant - together core thoughts and precepts underlying the unhelpful thoughts.
- This can be done based on the already completed Thought records, but you can also use a technique like the "downward arrow technique."
- Practice challenging and formulating helpful rules for living. Use this article to explore the client's rules for living.
- Create a list of all the helpful thoughts and have the client write them on a card to display in a prominent place, for example, to hang it up.
- If necessary, utilize alternative challenging techniques or cognitive techniques such as Downward Arrow Technique, Multidimensional Evaluation, Pie Chart Technique, Cost-Benefit Analysis, Probability Calculations, Role-Playing, Flash or Coping Cards, Imagery, and Imagery Rescripting.
- Examples of exercises and assignments for home:
- Fill out a Thought record daily, possibly with a reminder.
- Practice challenging thoughts and formulating helpful thoughts.
- If relevant, focus on creating helpful thoughts, core beliefs, and rules for living.
- Hang up cards with helpful thoughts or set reminders with helpful thoughts in the app.
- Practice imagery after formulating helpful thoughts.
Flexible time 20 min
Before starting behavioural experiments, it is important that your client is capable of formulating helpful thoughts. |
Before initiating behavioural experiments, it is crucial that your client is proficient in formulating helpful thoughts.
Session 5: 35 mins
- Discuss the assignments and encourage the client to continue filling out Thought records.
- Discuss the helpful thoughts and insights. Use the Thought record as a bridge to introduce the behavioural experiments.
- Explain behavioural experiments and why it is important to practice with different behaviours.
- Together, set up the first behavioural experiment. For example, based on the question "What would you do differently based on this helpful thought?" Both of you have the option to enter this in the NiceDay app.
- Examples of exercises and assignments for home:
- Continue practicing steps 1 to 3 of the Thought record.
- Conduct the behavioural experiment and fill in how it went.
Flexible time 20 min
|
Session 6 to completion 35 min
- Discuss how the first behavioural experiment went.
- Collaboratively generate more experiments for the client to practice (preferably as many as possible). You can find examples of behavioural experiments and guidelines on how to formulate them in the core intervention Behavioural Experiments.
- Examples of exercises and assignments for home:
- Carry out the experiments and record them in NiceDay.
- Carry out the experiments and record them in NiceDay.
Flexible time 20 min
|
Evaluate the effect of the Thought records, behavioural experiments, and insights gained after 6 sessions. If the intervention is effective, continue until the new cognitions and behaviours are more or less "anchored" and the treatment goals are (largely) achieved. If you notice that despite the efforts of the client and yourself, the therapy is not having sufficient effect, discuss this with the client and in the multidisciplinary team (MDT) meeting. Explore possible causes and make necessary adjustments to the therapy if needed.
🔁 Core intervention Relapse prevention
The goal of Relapse Prevention is to map out how someone can recognize and monitor potential relapse, identify their pitfalls, and provide them with tools to deal with symptoms or situations. This typically takes about 1-2 sessions.
Deepening core intervention relapse prevention
Flexible time - before the first relapse prevention session 5 min
|
Session (1 or 2 sessions) 35 min
- Reflecteer op de voortgang van de OMQ en SMQ en bespreek eventuele andere (ROM) vragenlijsten.
- Evaluate the treatment:
- Discuss the effect of the treatment.
- Which obstacles have been overcome and which ones are still present?
- Predict and normalize: It is normal to experience mood problems again in the future. Stress, fatigue, and/or changes in your life can play a role in this.
- Create the relapse prevention plan together:
- Make a list of situations and problems where relapse into "old behaviour" is likely.
- Have your client write down a strategy for each situation that can be applied in these specific situations.
- Exercises and assignments for home:
- Encourage your client to continue applying everything they have learned. This includes using the app, such as planning activities, recording moods, and using Thought records to challenge unhelpful thoughts.
- Ask your client to complete the relapse prevention plan.
Flexible time 20 min
|
📚 Use articles
Depending on the personal situation and issues of the client, you may choose to send supportive blogs. These blogs are written by professionals and individuals with lived experience and can be found on niceday.app. Examples include:
- Mind Reading: Can We Do It?
- Dealing with negativity
- Learn to relax
- Reluctance: how do you deal with it?
- How do you get into the pluses?
- Catastrophic Thinking
- Tips: Adjusting Rules for Living
- Affirmations against your anxious thought
- Did you know that your behaviour always has a function
- Make your own ground rules
- Do I have a realistic self image?
Sources
- https://www.ggzstandaarden.nl/zorgstandaarden/depressieve-stoornissen/behandeling-en-begeleiding/tweede-stap-psychologische-en-psychotherapeutische-behandelingen/psychotherapie
- Bockting, C., Rijsbergen, van G. & Huibers, M., Protocollaire behandeling van patiënten met een depressieve stoornis. In: Keijsers, G. P. J., Van Minnen, A., Verbraak, M., Hoogduin, C. A. L. & Emmelkamp, P., (2021). Protocollaire behandelingen voor volwassenen met psychische klachten.
- https://www.nvvp.net/stream/richtlijn-depressie-2013.pdf